Research
Anti-angiogenesis Gene Therapy
A central mandate to realize effective gene therapy is the ability to accomplish cell specific delivery. To this end, a range of vector targeting methods have been explored. Capitalizing on the in vivo delivery efficacy of adenoviral vectors (Ad), recent studies have highlighted the capacity of targeted Ad to accomplish cell selectivity in this stringent 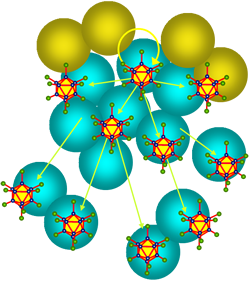 delivery context. Of note, a number of gene therapy models have clearly demonstrated the accrued value of vector targeting vis a’ vis improved indices of therapy and/or reduced toxicities. Indeed, such vector targeting paradigms have begun to be translated to the human clinical contexts, highlighting the compelling translational rationale to fully explore vector targeting strategies to address the central pharmacologic mandates of gene therapy. For Ad, recent work in several laboratories has identified the biologic dictates of vector hepatotropism, which has heretofore limited systemic delivery schemas. Based on this understanding, it has now been possible o “un-target” the liver thereby facilitating strategies designed to achieve cell specific gene delivery in the context of systemic vector administration. Of note, we have recently shown that such liver un-targeting strategies can synergize with described vector targeting methods such as those based upon restricting delivered transgene expression to target cells with a tissue/tumor selective promoter (“transcriptional targeting”.) The dramatic synergistic specificity gains noted with combination of these two approaches logically suggests that further gains may accrue additional targeting methods exploited in combination. In this regard, strategies have been proposed to target Ad based upon re-directing vector binding to target cell specific cell surface markers via antibody species. Such “transductional” targeting methods would offer potential synergies with the targeting methods we note above. This endeavor has been limited to this point, however, by the inability of available methods to accomplish capsid incorporation of functional antibody for targeting purposes. Recently, however, we have developed highly novel technologies to address this goal. First, we have developed a method to replace the native adenovirus fiber with a substitute chimera devoid of the native fiber’s knob binding domain. This maneuver eliminates native tropism and allows for the incorporation of a wider range of large/complex candidate targeting ligands. Second, we have demonstrated that the single domain antibody species derived from camelids (sdAb or “VHH”) possess the unique attributes allowing biologic capability with adenovirus capsid synthesis and assembly. In the aggregate, these two technologies now allow for the functional incorporation of antibody targeting species into the Ad capsid for the achievement of cell-specific targeting. The capacity to achieve such transductional targeting via a genetic capsid approach provides a vector engineering method fully commensurate with the mandates of human clinical translation. Of note, this additional level of targeting provides for potential synergies with the defined liver un-targeting and transcriptional vector targeting methods we have explored. In our recent studies, we have accomplished highly efficient and specific in vivo gene delivery to vascular endothelial cells exploiting liver un-targeting in combination with transcriptional targeting via the ROBO4 promoter. We presently seek to refine our targeting exclusively to tumor endothelial cells as a first step to establish key proof-of-principle with respect to targeting synergy gains. The recent identification of tumor endothelium markers specific to these target cells now provide an opportunity to advance this novel targeting approach. We hypothesize that transductional targeting via this axis will synergize with our liver un-targeting and ROBO4 transcriptional targeting to allow unprecedented levels of selectivity of in vivo gene delivery to tumor endothelium. delivery context. Of note, a number of gene therapy models have clearly demonstrated the accrued value of vector targeting vis a’ vis improved indices of therapy and/or reduced toxicities. Indeed, such vector targeting paradigms have begun to be translated to the human clinical contexts, highlighting the compelling translational rationale to fully explore vector targeting strategies to address the central pharmacologic mandates of gene therapy. For Ad, recent work in several laboratories has identified the biologic dictates of vector hepatotropism, which has heretofore limited systemic delivery schemas. Based on this understanding, it has now been possible o “un-target” the liver thereby facilitating strategies designed to achieve cell specific gene delivery in the context of systemic vector administration. Of note, we have recently shown that such liver un-targeting strategies can synergize with described vector targeting methods such as those based upon restricting delivered transgene expression to target cells with a tissue/tumor selective promoter (“transcriptional targeting”.) The dramatic synergistic specificity gains noted with combination of these two approaches logically suggests that further gains may accrue additional targeting methods exploited in combination. In this regard, strategies have been proposed to target Ad based upon re-directing vector binding to target cell specific cell surface markers via antibody species. Such “transductional” targeting methods would offer potential synergies with the targeting methods we note above. This endeavor has been limited to this point, however, by the inability of available methods to accomplish capsid incorporation of functional antibody for targeting purposes. Recently, however, we have developed highly novel technologies to address this goal. First, we have developed a method to replace the native adenovirus fiber with a substitute chimera devoid of the native fiber’s knob binding domain. This maneuver eliminates native tropism and allows for the incorporation of a wider range of large/complex candidate targeting ligands. Second, we have demonstrated that the single domain antibody species derived from camelids (sdAb or “VHH”) possess the unique attributes allowing biologic capability with adenovirus capsid synthesis and assembly. In the aggregate, these two technologies now allow for the functional incorporation of antibody targeting species into the Ad capsid for the achievement of cell-specific targeting. The capacity to achieve such transductional targeting via a genetic capsid approach provides a vector engineering method fully commensurate with the mandates of human clinical translation. Of note, this additional level of targeting provides for potential synergies with the defined liver un-targeting and transcriptional vector targeting methods we have explored. In our recent studies, we have accomplished highly efficient and specific in vivo gene delivery to vascular endothelial cells exploiting liver un-targeting in combination with transcriptional targeting via the ROBO4 promoter. We presently seek to refine our targeting exclusively to tumor endothelial cells as a first step to establish key proof-of-principle with respect to targeting synergy gains. The recent identification of tumor endothelium markers specific to these target cells now provide an opportunity to advance this novel targeting approach. We hypothesize that transductional targeting via this axis will synergize with our liver un-targeting and ROBO4 transcriptional targeting to allow unprecedented levels of selectivity of in vivo gene delivery to tumor endothelium.
Return To Top
One Health
One Medicine is the convergence of animal and human health. This trans-disciplinary approach employs novel interventions and new strategies to improve the health of all species by fostering ongoing collaborations and research.
Dogs suffer from cancer and chronic diseases just as humans. The therapeutic agents engineered in our laboratory are being used to treat canine companion animals at the University of Missouri, Columbia and Auburn University. As a result of these linkages, not only are these new therapies for dogs being implemented, but these studies provide an important and unique pathway to develop targeted therapies for intractable human cancers.
The center leadership is working to create better therapies and new strategies for treating and preventing both human and canine cancers. The team is also working to make these new therapies more widely available and build the critical infrastructure to make these novel therapies more widely accessible for humans and people’s pets with cancer.
By learning from research gathered from companion canines with natural cancers, the center aims to create a more rapid translation from the laboratory to the clinic.
Return To Top
SDAb Targeted CRAd
Virotherapy represents a powerful means to achieve targeted anti-tumor therapy which has been rapidly translated into human clinical trials. In this regard, the ability to engineer vial agents to replicate selectively in tumor cells constitutes the key facet of their design allowing anti-tumor selectivity to realize an optimized therapeutic index. Based on this concept, conditionally replicative adenovirus-based virotherapy agents (CRAds) have been applied for a wide range of localized neoplastic diseases. In selected instances, clear indices of clinical efficacy have been noted in human clinical trials. Indeed, our adenovirus-based virotherapy agent, “delta24”, has demonstrated preliminary efficacy in human clinical trials for glioma. Despite these promising findings in the context of locoregional disease, the application of CRAd agents to the major unaddressed clinical context of metastatic disease has been problematic. This is owing to the fact that tumor targeting, exclusively via replicative selectivity, does not address the specificity mandates of application for disseminated disease therapy. In this regard viral transduction of non-tumor targets constitutes the basis of dose-limiting toxicities. On the basis of this recognition, it is clear that configuring adjunctive tumor targeting mechanisms into CRAd design may serve to mitigate off-target transduction. Such improvements in tumor targeting would thus address the critical barrier which currently confounds application of adenovirus-based virotherapy for this desperate need area. To this point, tumor cell selectivity has been achieved with “transcriptional targeting” by restricting replication exclusively to tumor cells via replacement of native viral promoters with tumor selective promoters or viral genomic deletions. Controlling specificity at the level of viral replication, however, represents only one means by which specificity may be achieved. Viral tumor cell binding could represent an adjunctive means to achieve specificity, with the additional possibility of synergy of action. The approach to such “transductional targeting” requires the ability to functionally incorporate tumor binding ligands into the adenovirus capsid. To this end, capsid incorporation of peptide ligands has been explored by our group and others. Such targeting ligands, however, lack the optimized specificity and affinity advantages of antibody species. Until recently, the available antibody targeting species were too large to incorporate into the capsid of adenovirus. In addition, available antibody species lacked the stability required for compatibility with adenovirus biosynthesis and assembly. In this first regard, we have developed a novel “fiber replacement” method that allows viral capsid incorporation of large and complex candidate targeting ligands without adversely affecting viral structural dynamics. In the second regard, we have recently explored the utility of single domain antibodies derived from the camelid family (sdAb) for retargeting adenoviral vectors to tumor targets. On the basis of these breakthrough technologies, we hypothesize that the addition of sdAb-based transductional targeting will improve the tumor cell selectivity and efficacy of transcriptional restricted CRAd agents thereby achieving synergistic tumor targeting commensurate with the mandates of metastatic disease therapy.
Return To Top
Dendritic Cell Targeted Vaccine Vector
A number of critical advancements have predicated the possibility of dramatic efficacy improvements in antitumor approaches based upon immunotherapy. Characterization of valid tumor antigens, delineation of the functionality of key effector cells and definition of central immune regulatory pathways have, in the aggregate, provided a rationalized framework by which advanced immunotherapy strategies can be developed. Of note, recent human clinical studies exploiting retargeted T-effector cells have clearly demonstrated anti-tumor efficacies in on-going trials. In these instances, realization of enhanced therapeutic outcomes was achieved by directly exploiting these new biological insights into the immune system. In this context, a number of cancer vaccine approaches have sought to capitalize on new understandings of the central role played by the key immunoregulatory dendritic cell (DC). Such strategies have been applied to the context of breast cancer whereby anti-tumor immunization has been endeavored for defined tumor antigens. Of note, such approaches based upon direct antigen loading of DCs to enhance active immunization must now account for the diversity of DC-subsets, which embody distinct functionalities. In this regard, it has been proposed that targeting myeloid DCs may offer significant advantages as these cells are able to induce proper and oriented stimulation of T cell effector functions. In addition, targeting may also allow reduction in potential risks attendant to DC-based antigen loaded vaccines – induction of an autoimmune response and/or induction of tolerogenic DC-subtypes. Critical to the achievement of genetic targeting DC-subtypes is the availability of vector technology capable of efficient and selective gene delivery in the context of direct in vivo vaccination. To this end, we have developed methods to modify the tropism of adenoviral vectors (Ad) that allow the possibility of cell specific vector targeting. This has been feasibilized by two break-through technologies: (1) Methods to replace the native Ad capsid fiber binding protein with a fibritin chimera, and (2) The identification of a novel antibody targeting species compatible with Ad capsid incorporation. Such camelid-derived single domain antibody (sdAb) moieties embody unique attributes relevant to the pharmacologic mandates of DC-based vaccines. Most significantly, we now have the ability to target Ads with sdAb that recognize effector myeloid DCs. We now can accomplish the central field goal of effector-specific antigen loading of DCs as a novel strategy to optimize anticancer vaccination, which has not been heretofore possible via available vaccine vectors. These novel technologies offer synergistic possibilities with respect to developing an optimized Ad-based vector for selective DC transduction and for rapid bench-to-bed translation of such an approach. In this regard, one of the major limits to employment of Ad for human vaccine applications is the presence of anti-Ad preexisting immunity. To this end, the use of Ad derived from chimpanzees (ChAd) has recently provided a viable strategy to circumvent this key limiter. Of note, ChAd are technically compatible with human-based systems for vector upscaling and purification. Most importantly, they exhibit potency comparable to human Ad5-based vectors and have shown comparable capacity to generate protective immunity in pre-clinical models. Importantly, our methods of Ad retargeting to DCs are fully compatible with the ChAd methodologies. We are thus now uniquely positioned to develop DC-targeted ChAd, a highly novel vector species, which addresses the key mandates required to test our overall hypothesis.
Return To Top
|